For more than a decade, the Clinical Documentation Integrity (CDI) industry has been searching for “missed severity” in the same place, the medical record.
Millions have been invested in chart review resources, AI-driven query tools, and sophisticated documentation software, all built on one core assumption:
“If we can just find more diagnoses in the chart, we can capture more severity and improve CMI.”
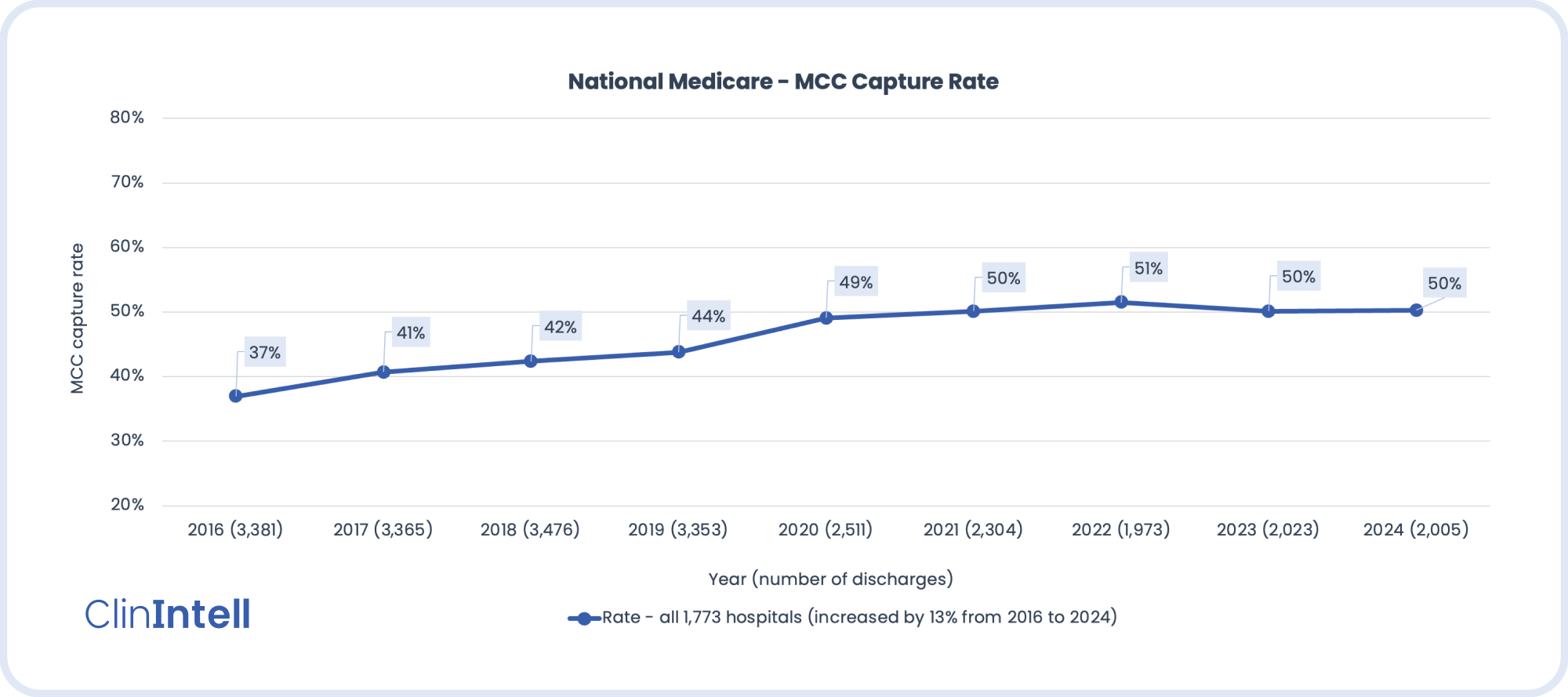
It worked for a while. But over time, national performance metrics like CC/MCC capture rates and Case Mix Index (CMI) have hit a wall. Despite major investments, hospitals are seeing diminishing marginal returns on their CDI efforts.
The reason is simple: we’ve been mining the same “source” for too long.
The Problem with the Current Model
The CDI industry’s entire economic engine runs on reviewing the medical record. Whether it’s a human reviewer or advanced technology, success depends on three fragile variables:
- Sufficient pertinent clinical information in the chart to justify a compliant query.
- Competency of the reviewer or algorithm to identify it.
- Scalability, the ability to apply this process across thousands of patient encounters.
That model was never designed to scale sustainably, and it never addressed the most important element: the source of the documentation itself, the physician. In fact, one might argue that the entire industry is not even slightly set up to engage physicians, let alone change their documentation practices.
After years of queries and nudges, physicians still largely view CDI as an external and/or administrative process rather than an intrinsic part of patient care. Without meaningful physician engagement, the quality of source data in the medical record hasn’t fundamentally changed. And if the input doesn’t improve, no amount of downstream technology will deliver new returns.
The Economics Behind the CDI Illusion
Since 2016, U.S. hospitals have spent billions on CDI programs, consultants, and technologies, most of which center on reviewing medical records to identify missed severity. Yet the national MCC capture rate has plateaued. CMI growth has slowed, even among hospitals adopting the most advanced CDI platforms and technologies.
The reality is stark: we’ve reached the point where every additional dollar invested in chart-based CDI yields less return than the one before. The marginal cost of finding “more severity” through manual reviews now outweighs the value gained.
Why Diminishing Returns Are Inevitable
When you only look for severity in the chart, you’re limited by what’s already there.
Here’s how that dynamic plays out in other industries, and why it’s a clear warning for healthcare.
1. Highway Analogy: Patching Without Repaving
Chart-focused CDI has been patching potholes (fixing documentation gaps one query at a time). But the road (documentation foundation) keeps deteriorating. At some point, the cost of patches exceeds the cost of re-paving the road (i.e., investing in a physician-engagement model that permanently improves source documentation).
2. Financial Analogy: Auditing Without Fixing
Hospitals have built multi-million dollar "audit departments" (CDI, AI tools) that keep auditing the books rather than correcting the entries. But if the accountants (physicians) keep making the same entries, the audits only find, not fix, the problem. You can audit forever, but until the underlying entries are corrected, the ledgers (medical records) won’t reflect true value.
Sustainable improvement requires changing the people who enter the information, not endlessly refining the process that checks it afterward. The following insights should raise red flags when pondering what the future of CDI looks like:
- You can’t scale an inherently unscalable model. Chart-based identification is reactive, not generative.
- You can’t automate poor source data, AI is only as good as the input it reads.
- The next era of CDI isn’t about finding more, it’s about fixing the source.
The Shift That Must Happen
The future of CDI isn’t about finding more or getting more proficient at finding more opportunities to query physicians, it’s about fixing the source. True improvement comes from understanding opportunities in your unique patient population and aligning physician documentation with an 80/20 approach to reflect that population’s true clinical complexity.
That’s why ClinIntell has taken a different approach. For over a decade, we’ve focused exclusively on CMI and claims-level analytics, building the most comprehensive understanding of documentation trends and population-level performance patterns in the country.
Our Population-Based CDI Assessment helps hospital leaders see:
- What the true severity documentation opportunity is within their own patient population.
- What investments in chart-based approaches have actually delivered over time.
- Whether their organization has already hit diminishing marginal returns on traditional CDI methods.
At a fraction of the cost of traditional consulting or technology assessments, we bring clarity to the question that should precede every new CDI investment:
Do you know what your real opportunity is or are you still flying blind?
Stop Mining the Chart. Fix the Source.
The CDI industry has spent years rearranging deck chairs on the Titanic (i.e., investing in more tools to analyze the same documentation). The only way forward is to focus on the source: the physicians, the data they create, and the patient populations they serve.
It’s time to stop squeezing the same sponge and start understanding the well it comes from. Only then can hospitals truly unlock the next era of sustainable CMI performance.
Schedule Your Free Population-Based Assessment

.svg)



.jpg)

.png)
.jpg)